Pneumonia is one of the most common and potentially serious respiratory infections worldwide. It affects people of all ages, but the risk of complications is higher in older adults, young children, and individuals with weakened immune systems. Understanding what pneumonia is, how it develops, how it is diagnosed, and how it is treated can help in early recognition and timely management.
This article provides a complete, easy-to-understand overview of pneumonia, including community-acquired and hospital-acquired pneumonia, symptoms, investigations, severity scoring systems, and evidence-based treatment approaches.
What Is Pneumonia?
Pneumonia is an infection of the lung tissue (lung parenchyma) that causes inflammation of the alveoli, which are the tiny air sacs responsible for oxygen exchange. When infected, these air sacs can fill with fluid or pus, making it difficult for oxygen to pass into the bloodstream.
Pneumonia can be caused by:
- Bacteria (most common cause)
- Viruses
- Fungi (especially in immunocompromised individuals)
The infection can range from mild to life-threatening, depending on the organism involved and the patient’s overall health.
Common Signs and Symptoms of Pneumonia
Symptoms of pneumonia can vary by age, severity, and cause, but commonly include:
- Fever and chills
- Productive cough with sputum
- Shortness of breath
- Chest pain that worsens with breathing or coughing
- Fatigue and weakness
Special Presentations to Watch For
- Older adults: Sudden confusion or altered mental status may be the first sign of pneumonia.
- Infants and young children: Rapid breathing, nasal flaring, grunting sounds, poor feeding, or bluish discoloration of lips and skin (cyanosis).
- Severe cases: Low oxygen levels, respiratory distress, or signs of sepsis.
Types of Pneumonia Based on Exposure
Correct classification of pneumonia is essential because it directly affects treatment decisions.
Community-Acquired Pneumonia (CAP)
Community-acquired pneumonia develops outside the hospital or within the first 48 hours of hospital admission.
Common causes include:
- Streptococcus pneumoniae (the most common bacterial cause)
- Viruses (influenza, COVID-19)
- Mycoplasma pneumoniae and Chlamydia pneumoniae (often cause mild “walking pneumonia”)
- Haemophilus influenzae (especially in COPD patients)
- Staphylococcus aureus (post-viral pneumonia)
- Legionella (older or immunocompromised patients; often associated with hyponatremia)
Hospital-Acquired Pneumonia (HAP)
Hospital-acquired pneumonia occurs 48 hours or more after hospital admission, in patients who were not infected at the time of admission.
These infections are usually caused by drug-resistant bacteria, such as:
- Pseudomonas aeruginosa
- MRSA (methicillin-resistant Staphylococcus aureus)
- Klebsiella
- E. coli
Because these organisms are more resistant, hospital-acquired pneumonia often requires stronger antibiotics and closer monitoring.
Pneumonia in Immunocompromised Patients
People with weakened immune systems are vulnerable to additional organisms, including:
- Pneumocystis jirovecii pneumonia (PCP) in HIV patients with CD4 counts <200
- Nocardia
- Non-tuberculous mycobacteria
- Fungal infections
These cases often require specialized testing and treatment.
How Pneumonia Is Diagnosed
Diagnosis is based on a combination of clinical assessment and investigations.
Initial Evaluation
- Review of symptoms and medical history
- Physical examination (listening to lung sounds)
- Measurement of oxygen saturation using pulse oximetry
Imaging
- Chest X-ray is the most important diagnostic test
- Lobar consolidation suggests bacterial pneumonia (e.g., Strep pneumoniae)
- Patchy interstitial infiltrates suggest viral or atypical pneumonia
Laboratory Tests
- Complete blood count (elevated white blood cells suggest infection)
- Sputum culture and Gram stain (before starting antibiotics)
- Blood cultures in severe cases
- Procalcitonin (may help distinguish bacterial vs viral infection)
- Viral PCR testing when viral pneumonia is suspected
- Arterial blood gas (ABG) in severe or hypoxic patients
Advanced Testing (Selected Cases)
- Bronchoscopy for severe or non-responsive cases
- Urinary antigen tests for Legionella
- HIV testing when immunodeficiency is suspected
Pneumonia Severity Assessment
Severity scoring systems help determine whether a patient can be treated at home or needs hospitalization or ICU care.
qSOFA Criteria (Quick Assessment)
Used for rapid risk assessment:
- Respiratory rate ≥22/min
- Altered mental status
- Systolic BP ≤100 mmHg
A score ≥2 indicates higher risk and need for urgent care.
CURB-65 Score (Pneumonia-Specific)
- Confusion
- Urea >20 mg/dL
- Respiratory rate ≥30/min
- Blood pressure <90/60 mmHg
- Age ≥65 years
Interpretation:
- 0–1: Outpatient treatment
- 2–3: Hospital admission
- ≥4: ICU consideration
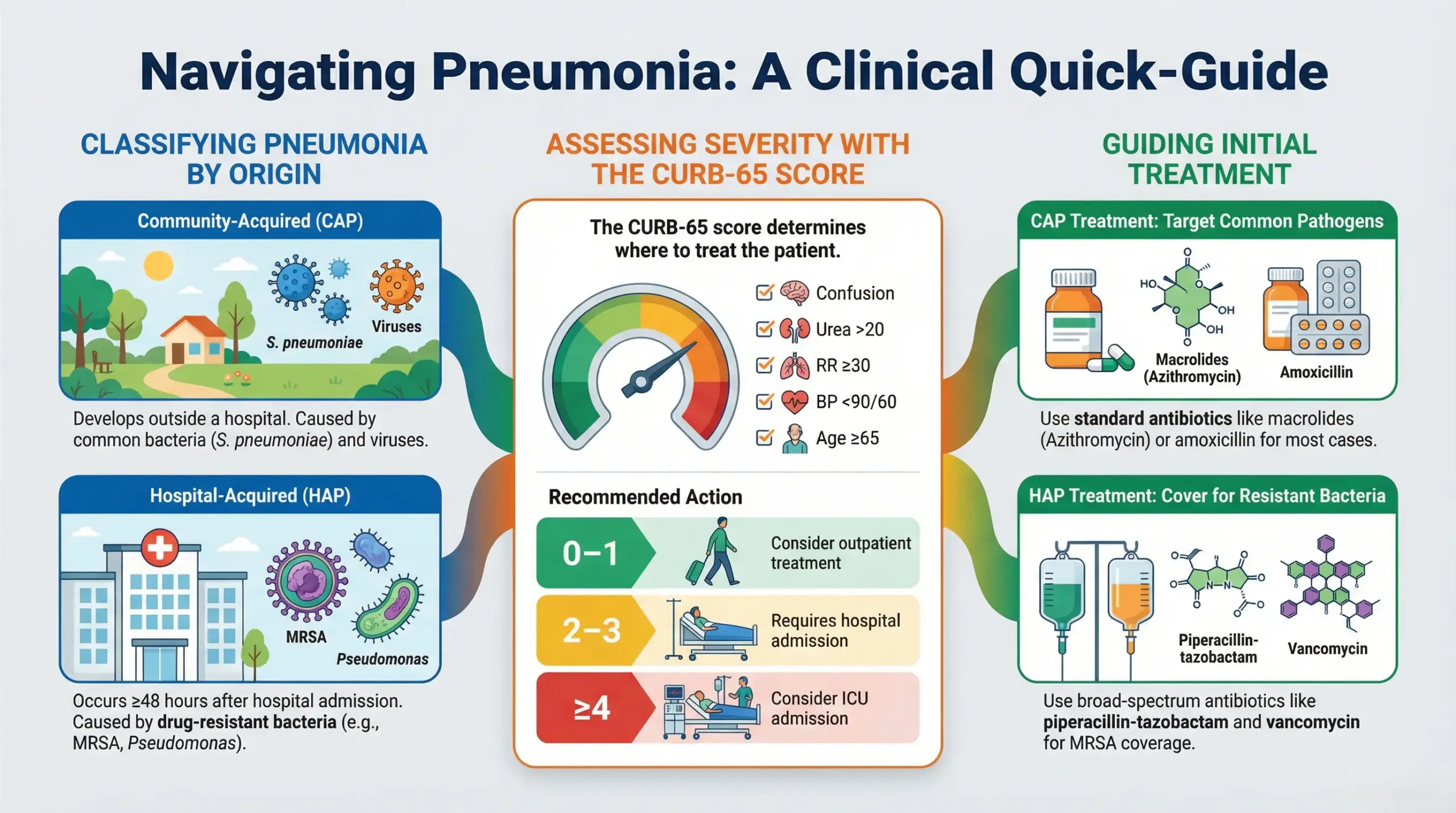
Treatment of Pneumonia
Treatment depends on the type, severity, and cause of pneumonia.
Community-Acquired Pneumonia
- Mild cases (outpatient):
- Azithromycin, doxycycline, or clarithromycin
- Azithromycin, doxycycline, or clarithromycin
- Moderate cases (hospitalized):
- Amoxicillin + macrolide
- OR respiratory fluoroquinolone
- Severe cases (ICU):
- Third-generation cephalosporin + respiratory fluoroquinolone
- OR beta-lactam + macrolide
Hospital-Acquired Pneumonia
- Broad-spectrum antibiotics targeting resistant organisms:
- Piperacillin-tazobactam
- Vancomycin (for MRSA)
- Carbapenems for resistant cases
- De-escalation once cultures identify the organism
Role of Steroids
Steroids are not routinely used, but may be considered in severe community-acquired pneumonia to reduce inflammation and complications.
Supportive Care and Recovery
Supportive measures play a crucial role in recovery:
- Oxygen therapy when needed
- IV fluids in hospitalized patients
- Incentive spirometry to improve lung expansion
- Adequate hydration to thin respiratory secretions
- Sitting upright and frequently deep breathing
Recovery may take weeks, and fatigue can persist for up to a month.
Preventing the Spread of Pneumonia
To reduce transmission and complications:
- Cover your mouth and nose when coughing or sneezing
- Wash your hands frequently
- Avoid close contact when ill
- Complete prescribed medications fully
Vaccination and Prevention
Pneumococcal vaccination is recommended for:
- Adults aged 65 and older
- Immunocompromised individuals
- People with chronic heart, lung, liver, or kidney disease
Vaccination significantly reduces the risk of severe pneumonia and complications.
Final Thoughts
Pneumonia is a complex but manageable disease when approached systematically. Early diagnosis, appropriate classification, and timely treatment significantly reduce complications and mortality.
If respiratory symptoms persist or worsen, timely medical evaluation is essential. You may also consult healthcare professionals online through platforms like the MedIQ app for guidance and early intervention.
Disclaimer:
This content is for general awareness only and is not a substitute for medical advice. Always consult a qualified healthcare professional for proper diagnosis and treatment, especially if symptoms worsen

